Bioelectrical Impedance Anaylisis a Review of Principles and Applicaitons
Loss of body weight and depletion of fat complimentary musculus mass are common and serious bug in patients with chronic obstructive pulmonary disease (COPD) irrespective of the degree of airflow limitation [1–3]. Malnutrition in COPD has been associated with systemic inflammation, cachexia, anorexia, skeletal muscle dysfunction, dyspnoea, reduced health status, enhanced risk of exacerbations and increased bloodshed [4–8]. Consequently, current COPD guideline recommendations past Gilt (Global Initiative for Chronic Obstructive Lung Disease) consider nutritional monitoring an important office of routine evaluation of COPD patients [9].
Surrogate measures such equally the well-known Body Mass Alphabetize (BMI) give no indication of body limerick, musculus mass or nutritional land. Thus, malnutrition requiring intervention can be in spite of a normal to high BMI. These patients are normally not detected by subjective global assessment of nutritional status. In the case of COPD, it has been recognized that information technology is low fatty-costless mass (FFM) further differentiated into body cell mass (BCM) and extra cellular mass (ECM) rather than depression BMI that should be considered as a critical parameter of disease severity and prognosis [x, 11].
Different methods are used for nutritional assessments beyond BMI, such as bioelectrical impedance analysis (BIA), skin-fold anthropometry and dual-energy Ten-ray absorptiometry (DEXA) [12–14]. BIA is a simple, inexpensive, quick and non-invasive technique for assessing body composition and its changes over fourth dimension. BIA is largely used in clinical trial settings and in that location is a whole series of literature on the theory and methodology of several different BIA techniques [fifteen–18]. Surprisingly enough, however, at that place is considerable lack of information on the practical aspects of BIA for those primarily interested in learning how to apply and translate this method in practice. Thus, BIA withal is an underused and underestimated tool for nutritional assessment in principal care. This tin exist farther explained by the fact that the costs of BIA are currently non ever refundable [12] and that there are no guidelines outlining the methods for assessing malnutrition in patients with COPD [nine, 19].
BIA analysis is only and effectively complemented by bioelectrical impedance vector analysis (BIVA), which is contained of hydration status and can be used as a quality control measure for right interpretation of BIA results [20, 21]. BIVA is a pattern analysis of impedance measurements (resistance and reactance) plotted as a vector in a coordinate system [21]. Reference values adjusted for age, BMI and gender are plotted equally so-chosen tolerance ellipses in the coordinate organization. On this footing, a statement can be made with regard to water residual (normo-, hypo-, hyperhydration) and trunk cell mass (nutritional condition) [14].
The purpose of this commodity is to provide some guidance on the utilise of BIA/BIVA with item attention to applied considerations. It reflects a decade of our own practical experience of using single-frequency BIA combined with BIVA with a focus on COPD patients. Here, we briefly describe the basic principles, feasibility and limitations of BIA/BIVA methodology and provide applied tips and recommendations for appropriate conduct and analysis of the measurements. We have aimed to provide a simple, structured and practice-oriented arroyo to the interpretation and analysis of BIA/BIVA results using feature examples seen in patients with COPD.
Basic principles
Bioelectrical impedance analysis (BIA)
BIA is a method for estimating trunk limerick. The principle of BIA is to make up one's mind the electrical impedance of an electrical current passing through the body [15]. The electric impedance (Z) consists of two components, resistance (R) and reactance (Xc). Reactance is a mensurate of BCM and resistance a measure of total trunk h2o [15, 22]. From the determined impedance a number of BIA parameters tin be estimated [xx]:
Body cell mass (BCM)
-
consists of all cells that have an effect on metabolism (east.g. musculus, internal organs, nervous system)
-
key factor when assessing the nutritional status of a patient
-
↑: e.one thousand. good training status, intracellular h2o retention
-
↓: eastward.1000. malnutrition, cachexia, dehydration
BCM %
-
percentage of BCM in FFM
-
for differential diagnosis of BIA changes: changes in the same way as BCM
-
measure of individual nutritional status and concrete fettle level
-
↑: east.g. skillful training condition
-
↓: e.k. malnutrition
Actress cellular mass (ECM)
-
mainly extracellular water
-
increase or decrease mostly due to increased extracellular water retention or a loss of extracellular water
-
↑: east.thousand. extracellular h2o retentivity (due east.g. oedema)
-
↓: e.g. extracellular loss of water (east.g. diuretics)
Fat-gratuitous mass (FFM)
-
everything that is non body fat, consists of BCM and ECM
-
↓: elderly people, chronic diseases
Fat mass (FM)
-
is indirectly determined from trunk weight minus FFM
Stage angle
-
ane of the best indicators of jail cell membrane function
-
can be regarded as a marker of training and nutritional status
-
↑: e.chiliad. athletic ramble type, good nutritional status (of BCM cells)
-
↓: due east.g. poor preparation condition, poor nutritional status (of BCM cells)
Total trunk water (TBW)
-
↑: eastward.g. high portion of muscle, water retentiveness (e.g. oedema)
-
↓: e.g. small portion of muscle, dehydration/exsiccosis
The strengths and limitations of dissimilar BIA methods (due east.g. single frequency, multi-frequency, segmental BIA) have been extensively reviewed [fifteen, 16, 18, 23–25].
Our experience is based on single frequency BIA (50 kHz); the software package we use (NUTRIPLUS from Data Input GmbH) includes BIVA and adapted reference values.
Detailed instructions for performing BIA measurements tin can be found elsewhere [17, 18]. To give a cursory description hither, unmarried frequency BIA commonly involves the placing of two distal electric current or signal-introducing electrodes on the dorsal surfaces of the paw and foot close to the metacarpal-phalangeal and metatarsal-phalangeal joints, respectively. The two voltage sensing electrodes are applied at the pisiform prominence of the wrist and between the medial and lateral maleoli of the ankle. The impedance analyzer delivers a constant alternate current at a stock-still 50-kHz frequency via the distal electrodes and detects the driblet in voltage via the proximal electrodes. The measured resistance and reactance are displayed by the analyzer [18].
Factors impacting BIA results [16, 18, 20, 23, 25]:
- 1.
weight and height (should be measured direct past the investigator)
- 2.
position of the body and limbs (supine position, arms abducted at to the lowest degree 30°, legs abducted at approximately 45°)
- 3.
consumption of food and beverages (no beverages for at least 12 hours previously, fasted state for at to the lowest degree 2 hours)
- iv.
moderate to intense level of physical activity/practise before BIA measurements (final practise at least 12 hours previously)
- five.
medical conditions and medication that have an bear upon on the fluid and electrolyte rest; infection and cutaneous affliction that may change the electrical transmission between electrode and skin
- six.
environmental conditions (e.g. ambient temperature)
- 7.
individual characteristics (e.k. skin temperature, sex, age, race)
- eight.
indigenous variation
- 9.
not-adherence of electrodes, utilize of wrong electrodes, loosening of cablevision clip, interchanging of electrodes
BIA parameters are largely dependent on the patient's hydration status. BIA enables the above mentioned parameters to be determined in subjects without significant fluid and electrolyte abnormalities [xv].
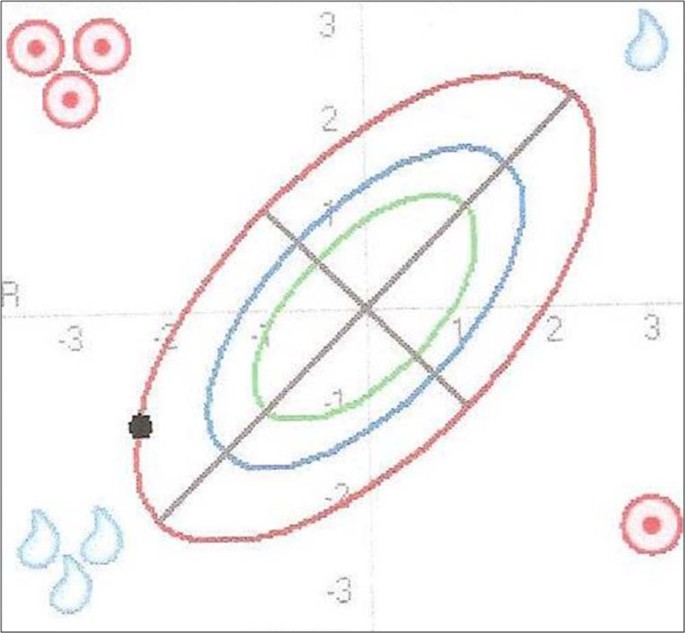
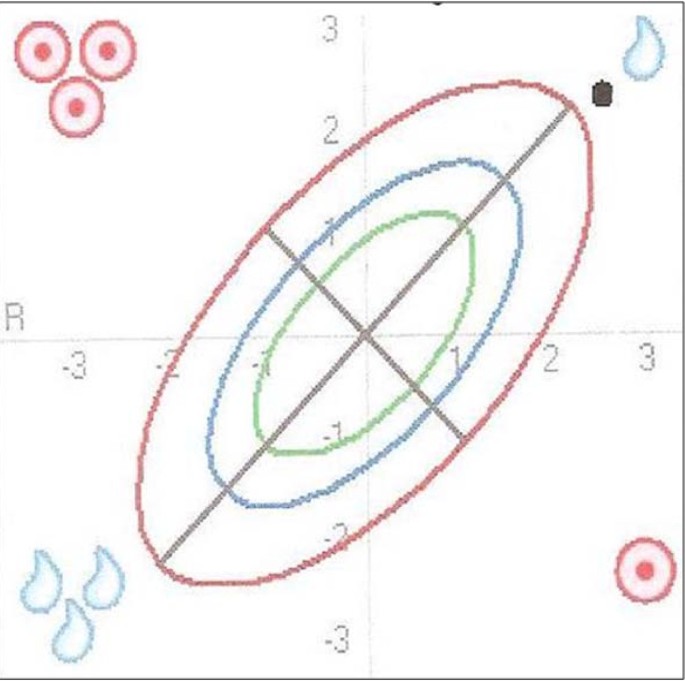
BIVA (bioelectrical impedance vector analysis)
BIVA as an integrated part of BIA measurement is a elementary, quick and clinically valuable method for assessing fluid status (TBW) and body cell mass (BCM). This method plots the directly impedance measurements resistance R and reactance Xc as a bi-variate vector in a nomogram (Effigy one) [21]. Reference values adapted for historic period, BMI and gender are plotted equally so-called tolerance ellipses in the same coordinate system. Iii tolerance ellipses are distinguished, corresponding to the lth, 75th and 95thursday vector percentile of the healthy reference population [22, 26]. Values outside of the 95thursday percentile are considered abnormal. Based on the position of the measurement signal in the BIVA nomogram, the sex-, age-, BMI- and race-adjusted nutrition/training and hydration status can be read off at a glance [21]. As shown in Effigy one, values located outside the 95th percentile in the following four quadrants point to the post-obit conditions [xx]: a) right upper quadrant due east.thou. exsiccosis b) left lower quadrant eastward.chiliad. oedema c) correct lower quadrant e.thou. malnutrition d) left upper quadrant e.g. proficient grooming status.
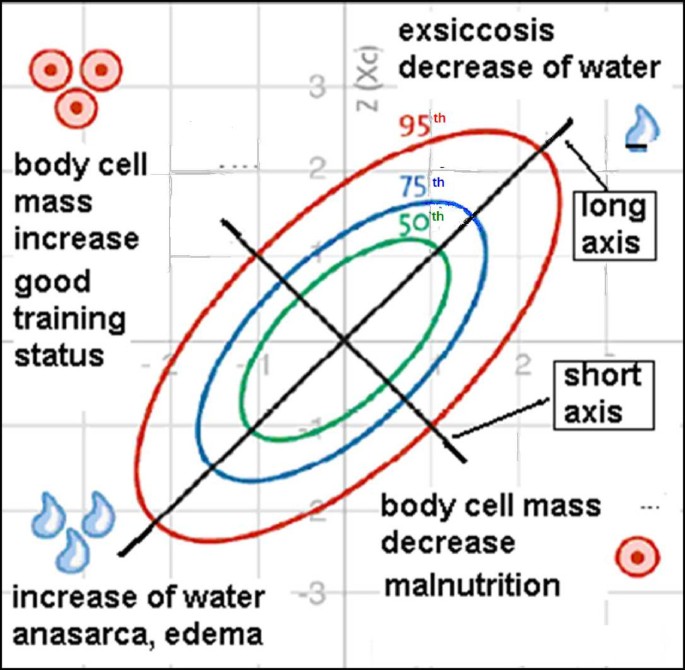
Interpretation of the BIVA nomogram. Historic period, BMI and gender adjusted reference values are plotted as so-called tolerance ellipses in the coordinate system. Iii tolerance ellipses are distinguished, respective to the lth, 75th and 95thursday vector percentile of the healthy reference population. Values outside of the 95thursday percentile are considered abnormal. Values located above the long axis (/) indicate an increment in trunk cell mass (BCM), values below the long axis indicate a subtract in BCM. Values located in a higher place the brusque axis (\) indicate a loss of water and values beneath the short axis betoken increased water retention. Values located outside the 95th percentile in the post-obit four quadrants point to the following atmospheric condition: a) right upper quadrant east.thousand. exsiccosis b) left lower quadrant e.g. oedema c) right lower quadrant eastward.grand. malnutrition d) left upper quadrant east.g. good training condition (modified with permission from Data-Input GmbH).
Applications of BIA/BIVA and interpretation of body composition
We present below some examples of characteristic BIA findings in COPD patients with their interpretation:
- 1.
Normal finding
- 2.
Malnutrition in a COPD patient with overweight
- 3.
Cachexia
- 4.
Oedema due to right eye failure
- v.
Anorexia
From personal experience, follow-up measurements (examples 2-5) should be performed every 4 weeks for overweight patients and every 8-12 weeks for all other cases [27]. Even so, this is a determination that must exist taken on an private basis.
1. Normal finding
Patient: female, 61.1 kg, BMI 22.7, 64 years old, mild COPD (GOLD stage I) [9].
Interpretation: With a BMI of 22.seven this patient is of normal weight. The measurement point in the BIVA nomogram (Figure ii) lies within the 50th tolerance ellipse and thus indicates normal findings. The TBW, ECM, trunk fatty, BCM, BCM % and phase bending values listed in table 1 are inside the normal range.
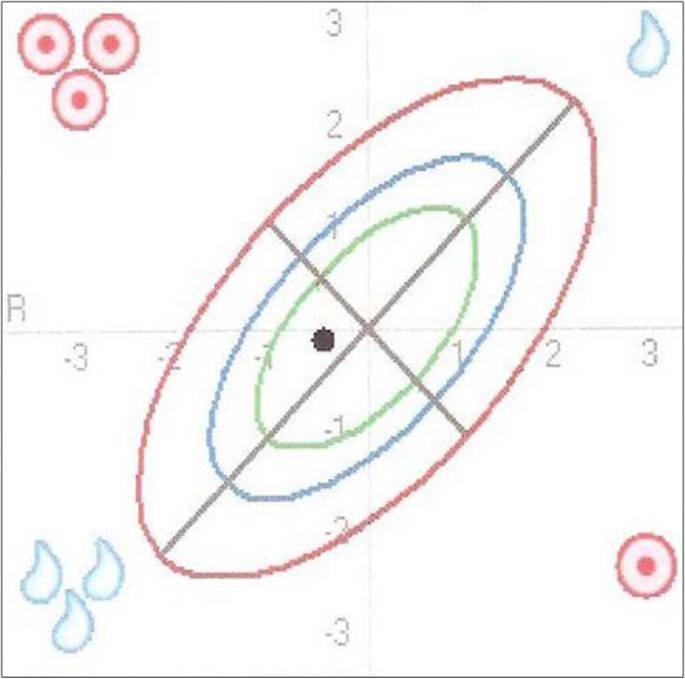
Normal finding as illustrated in the BIVA nomogram. The position of the measurement point in the BIVA nomogram inside the 50th tolerance ellipse (range of normal values) indicates a normal finding.
Decision: All values in the table are inside the normal range and the measurement point in the BIVA nomogram lies within the 50th tolerance ellipse.
2. Malnutrition in an obese COPD patient
Patient: female person, 90 kg, BMI 31.v, 73 years old, astringent COPD (GOLD stage Iii)
Interpretation: With a BMI of 31.5 this patient is obese. The measurement point in the BIVA nomogram (Figure iii) in this patient is well below the line of normal BCM values (long centrality) and in a higher place the line of normal TBW values (brusk axis) betwixt the 75th and the 95th tolerance ellipse. The position of the measurement point in the lower right quadrant points to malnutrition.
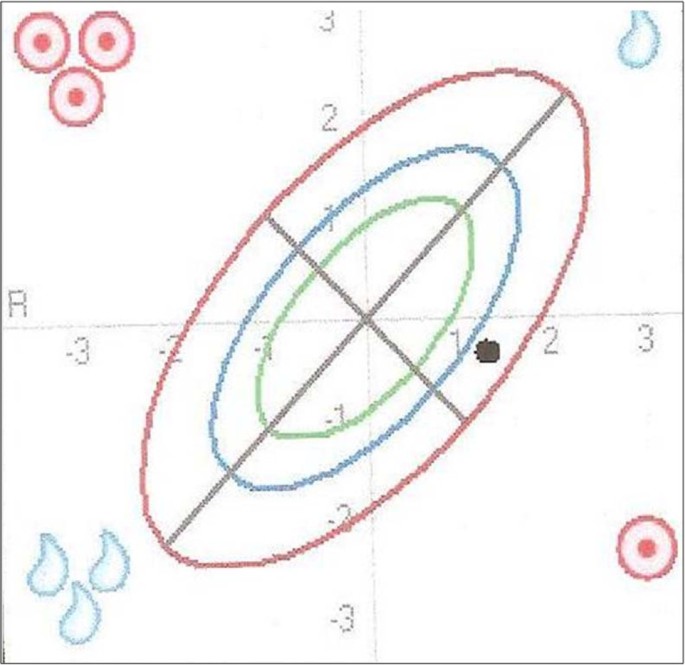
Malnutrition in an obese COPD patient as illustrated in the BIVA nomogram. The position of the measurement betoken in the BIVA nomogram is below the line of normal BCM values (long axis) and above the line of normal TBW values (short axis) between the 75th and 95th tolerance ellipse. The position in the lower right quadrant indicates malnutrition.
The BIA parameter values listed in tabular array 2 can be interpreted as follows: The fat mass lies above the normal range in line with the increased BMI. BCM lies inside the normal range. At first sight this does not fit in with the finding of the BIVA nomogram, which indicates malnutrition. The fact that the calculated BCM is within the range of normal values here may be explained every bit follows: It needs to be considered that BCM is dependent on the patient's fluid status (TBW). This ways that a BCM within the normal range does not necessarily mean a normal nutritional condition merely may as well be due to increased TBW. The following 2 BIA parameters are helpful in cartoon a distinction: BCM % and phase angle, which are usually altered along the same lines as BCM. In this instance TBW is increased and the BCM % and phase angle are below the range of normal values. This indicates that BCM is really reduced. BCM therefore merely appears to prevarication within the range of normal values because of the increased TBW. In dissimilarity to this somewhat complex interpretation of the calculated BIA values, the suspected diagnosis of malnutrition tin be established at a glance by BIVA. In improver, information technology is confirmed that the calculated BCM is too high considering of the increased TBW (position of the measurement point in the BIVA nomogram above the line of normal TBW values).
Conclusion: Despite the presence of obesity the patient is exhibiting malnutrition. The position of the measurement betoken in the BIVA nomogram in the right lower quadrant betwixt the 75thursday and the 95th tolerance ellipse provides an indication for the suspected diagnosis of malnutrition.
3. Cachexia
Patient: male, 45 kg, BMI xvi.7, 62 years former, severe COPD (GOLD stage 3)
Interpretation: With a BMI of xvi.vii the patient is underweight. The measurement point in the BIVA nomogram (Figure four) in this patient is far below the line of normal BCM values (long axis) and well in a higher place the line of normal TBW values (brusk axis), far exterior the 95thursday tolerance ellipse. The position of the measurement indicate in the lower right quadrant points to malnutrition in the form of cachexia.
Cachexia every bit illustrated in the BIVA nomogram. The position of the measurement point in the BIVA nomogram is far below the line of normal BCM values (long axis) and well above the line of normal TBW values (brusk axis) far exterior the 95th tolerance ellipse. The position in the lower right quadrant points to cachexia.
The BIA parameter values listed in table iii can exist interpreted as follows: The fatty mass lies below the normal range in line with the reduced BMI. The calculated values for BCM und TBW are reduced. It needs to exist considered equally regards the reduced BCM value that BCM is dependent on the patient'southward fluid status (TBW). This means that a reduced BCM does not necessarily point to malnutrition simply may as well be due to a low TBW. The BIA parameters BCM % and stage angle are again helpful for drawing a stardom, every bit they are usually contradistinct along the aforementioned lines as BCM. The values for BCM % and phase bending are reduced, which indicates an really reduced BCM or malnutrition. In this example as well BIVA provides a more than efficient assessment of the nutritional condition than the calculated BIA parameters.
Determination: All the values listed in the tabular array are beneath the normal range and the measurement signal in the BIVA nomogram is outside the 95th tolerance ellipse in the lower right quadrant. This indicates astringent malnutrition in the grade of cachexia. The assessment of the BIVA nomogram is sufficient for the suspected diagnosis of cachexia.
4. Oedema due to right heart failure
Patient: female, 105.6 kg, BMI 38.8, 78 years onetime, COPD Golden stage II
Estimation: With a BMI of 38.8 the patient is overweight. The measurement signal in the BIVA nomogram (Effigy 5) in this patient is above the line of normal BCM values (long axis) and well beneath the line of normal TBW values (brusque axis) on the 95th tolerance ellipse. The position of the measurement betoken in the lower left quadrant points to water retention in the form of oedema.
Oedema due to right eye failure as illustrated in the BIVA nomogram. The position of the measurement point in the BIVA nomogram is above the line of normal BCM values (long axis) and well below the line of normal TBW values (short centrality) on the 95th tolerance ellipse. The position in the lower left quadrant indicates the presence of increased water memory.
The BIA parameter values listed in table 4 tin be interpreted as follows: Body fat mass lies above the normal range in line with the increased BMI. The determined TBW is increased and the calculated BCM lies in the upper range of normal. These findings are consistent with the position of the measurement point above the line of normal BCM values and below the line of normal TBW values in the lower left quadrant. With the derived normal BIA value for BCM it needs once once more to be taken into business relationship hither that BCM is dependent on the patient's fluid status (TBW). This ways that a BCM within the normal range does not necessarily betoken an actually normal BCM or normal nutritional condition merely may also announced normal due to an increased TBW. The BIA parameters BCM % and phase bending, which are commonly altered along the aforementioned lines every bit BCM, in this instance prevarication in the lower range of normal, and then that information technology may be causeless that the BCM is really in the normal range. In improver to the increased TBW, ECM is also markedly increased, indicating oedema. The suspicion of oedema is established at a glance with BIVA. BIVA confirms simply and rapidly the calculated BIA values BCM and TBW. The suspicion of oedema was confirmed on physical examination of the legs.
Conclusion: The values listed in the table for TBW and ECM are outside the normal range and the measurement point in the BIVA nomogram is on the 95thursday tolerance ellipse in the lower left quadrant, indicating oedema. The determined BCM is in the upper range of normal and the measurement point in the BIVA nomogram is to a higher place the line of normal BCM values. The position of the measurement point in the nomogram provides an indication for the suspected diagnosis of oedema.
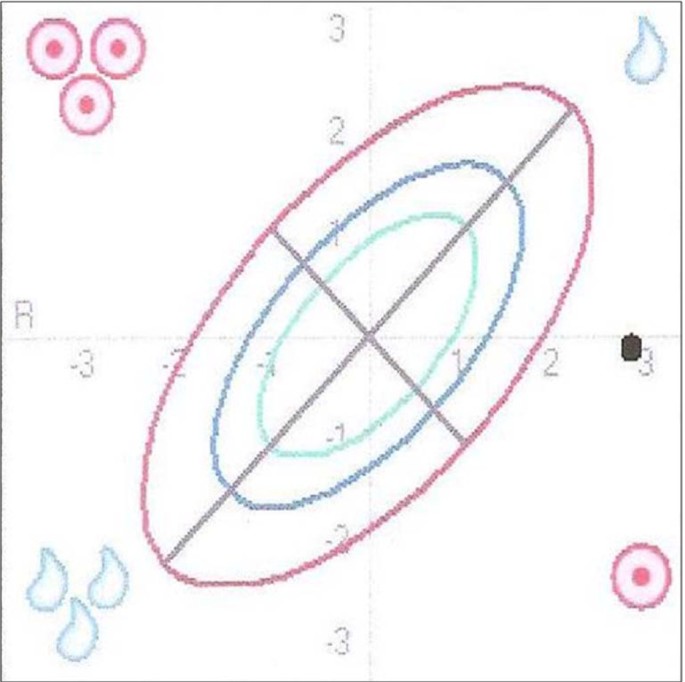
5. Anorexia
For the full general differential diagnosis of underweight we nowadays a female patient with anorexia: female, 34.1 kg, BMI 18.4, 41 years old, anorexia (unintentional loss of appetite).
Interpretation: With a BMI of 18.four the patient is underweight. The measurement point in the BIVA nomogram (Effigy 6) lies about on the line of normal BCM values (long axis) and far above the line of normal TBW values (brusk axis) outside the 95th tolerance ellipse. The position of the measurement bespeak in the upper right quadrant points to the presence of anorexia.
Anorexia as illustrated in the BIVA nomogram. The position of the measurement signal in the BIVA nomogram is almost on the line of normal BCM values (long axis) and far above the line of normal TBW values (brusk axis) exterior the 95th tolerance ellipse. The position in the upper right quadrant points to the presence of anorexia.
The BIA parameter values listed in table 5 can exist interpreted every bit follows: Body fat mass is reduced in line with the depression BMI. TBW is markedly reduced and BCM also is decreased. With the reduced BCM it needs to exist kept in mind here that BCM is dependent on the patient's fluid status (TBW). This means that a lower BCM may also appear reduced due to a lower TBW. The BIA parameters BCM % and phase bending which are helpful in drawing a stardom and which are usually altered in the same fashion every bit BCM, in this case lie in the upper tertiary of the normal range. This indicates that BCM is normal and that the calculated value was too low only because of the low TBW. BIVA confirms the suspicion raised past the BIA values that the calculated BCM was likewise depression because of the reduced TBW. Again, the suspected diagnosis of anorexia tin can be established more efficiently and more reliably by BIVA.
Conclusion: The patient exhibits a markedly reduced BMI, decreased body water and a normal BCM in the form of anorexia. The position of the measurement point in the nomogram in the upper right quadrant exterior the 95th tolerance ellipse provides an indication for the suspected diagnosis of anorexia.
Source: https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-10-35
Posting Komentar untuk "Bioelectrical Impedance Anaylisis a Review of Principles and Applicaitons"